Impact of AI on Maternal Mortality: Global Disparities and Healthcare Innovations
Descriptive statistics reveal significant disparities in maternal mortality rates between developed and developing countries. While AI adoption in maternal healthcare remains uneven globally, developed nations show higher integration. Key indicators suggest AI-driven innovations could have a substantial impact on reducing maternal mortality, particularly in resource-limited settings. Pairwise correlations highlight the positive relationship between AI adoption and lower maternal mortality rates. The analysis underscores the potential of AI technology in improving maternal health outcomes, especially in developing countries.
Descriptive statistics
Table 1 presents the descriptive statistics across all countries and separately for developed and developing nations. The global maternal mortality ratio (MMR) averages 55.96 deaths per 100,000 live births, with substantial variation (Std. Dev. = 157.27), reflecting disparities in healthcare access and maternal health outcomes. Developed countries report a significantly lower average MMR of 12.03 deaths per 100,000 live births (Std. Dev. = 12.06), suggesting minimal variation and relatively uniform healthcare quality. In contrast, developing countries experience substantially higher maternal mortality, averaging 109.49 deaths per 100,000 live births (Std. Dev. = 222.51), with more significant variation. This wide disparity may indicate inconsistent maternal healthcare access and higher risk factors in resource-limited settings.
Globally, the adoption of AI-driven robotics in maternal healthcare remains uneven. The average flow of industrial and service robots is 2,094.33 units, while the stock (cumulative AI adoption) reaches 16,068.02 units, with significant cross-country variation (Std. Dev. = 9,534.13 and 62,002.22, respectively). Developed countries exhibit higher AI integration, with an average robot flow of 2,673.55 units and a stock of 23,941.95 units, reflecting advanced digital healthcare infrastructure and greater technological investments. However, developing countries show substantially lower AI adoption, with an average robot flow of just 1,388.41 units and a stock of 6,471.66 units, indicating a lag in AI-driven healthcare innovation and limited technological resources.
Key indicators that reduce maternal mortality, such as healthcare access and socioeconomic indicators, are significantly lower in developing countries, while deprivation factors remain high. The low levels of AI adoption, insufficient infrastructure, and weak health systems suggest that AI-driven maternal health improvements could be particularly impactful in developing countries despite potential labor market challenges.
The pairwise correlation results in Table 2 reveal several significant relationships between AI adoption, healthcare factors, and maternal mortality rates. The negative correlation between industrial and service robotics (flow and stock) and MMR suggests that advancements in AI technology contribute to lower maternal mortality rates. AI technology improves maternal health outcomes through enhanced diagnostics, efficient treatment methods, streamlined healthcare processes, and better resource allocation. However, inadequate healthcare infrastructure and limited human capital investments may hinder AI’s effectiveness in reducing maternal mortality, particularly in resource-constrained settings.
Healthcare access and health expenditure also play a crucial role. The health access index and health expenditure correlate negatively with MMR, confirming their importance in reducing maternal mortality. In contrast, out-of-pocket (OOP) health expenditure positively correlates with MMR, indicating that higher personal healthcare costs limit access, particularly for low-income populations, leading to poorer maternal health outcomes. The negative correlation between OOP and overall health indicators supports the argument that greater financial burdens reduce healthcare accessibility.
Pre-existing health conditions significantly influence maternal mortality, as shown by the positive correlation between comorbidities and MMR. This finding underscores the heightened risks faced by pregnant women with underlying health conditions, aligning with previous research on maternal health vulnerabilities. Additionally, key socioeconomic and healthcare factors affect maternal mortality rates. Greater access to obstetric care, improved infrastructure, and affluent socioeconomic conditions negatively correlate with MMR, reinforcing their role in improving maternal health outcomes. Conversely, poor socioeconomic conditions and higher fertility rates are positively correlated with MMR, indicating that economic hardship and high birth rates contribute to increased maternal mortality.
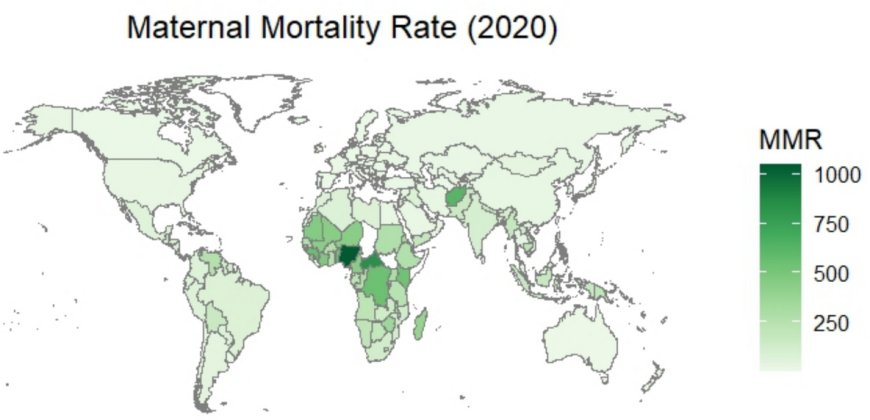
The key determinants of maternal mortality are strongly correlated with each other and, more importantly, with AI robotics indicators, raising concerns about multicollinearity in regression models. To address this, the subsequent analysis emphasizes bivariate approaches to ensure more reliable estimations. As shown in Fig. 1, maternal mortality rates remained a major global health concern in 2020, with significant country and regional disparities. Many low- and middle-income countries faced weak healthcare systems, limited access to skilled providers, inadequate infrastructure, and high fertility rates, all of which contributed to increased maternal mortality rates. Additionally, high poverty levels and poor maternal nutrition further exacerbated maternal health risks. The COVID-19 pandemic worsened the already fragile healthcare systems in many African countries, leading to deteriorating maternal health outcomes. In contrast, high-income countries—particularly in Europe, East Asia, and North America—maintained significantly lower maternal mortality rates in 2020.
Figure 2 illustrates the global distribution of robotic flows (upper map) and stocks (lower map) in 2020. Countries without available data are omitted. The global AI flow showed significant progress, reflecting the growing integration of AI across healthcare, manufacturing, banking, and education. However, AI adoption varied widely across regions, influenced by technological infrastructure, investment levels, and digital preparedness. High-income countries, particularly in East Asia, North America, and Europe, recorded the highest AI inflows, driven by advanced digital infrastructure and substantial R&D investments. In East Asia alone, AI flow exceeded 150,000 units, with many countries expanding AI adoption in healthcare to enhance diagnostic accuracy, personalize treatment, and streamline clinical workflows. In contrast, low-income countries, particularly in sub-Saharan Africa and South Asia, saw limited AI adoption in 2020. While some nations, such as South Africa and Kenya, have made strides in AI adoption—notably in agriculture and healthcare—overall AI flow in Africa remains low.
Countries with the highest AI stocks were predominantly high-income nations in North and Central America, Europe, and East Asia, where strong digital infrastructure and significant R&D investments drive AI expansion. In these regions, AI stocks are concentrated in healthcare, autonomous vehicles, defense, and finance, reflecting their strategic importance.
Difference-in-Difference estimations
The year 2000 marked a milestone in AI and robotics with the creation of Kismet, the first robot designed to simulate human emotions. Two years later, in 2002, the release of the first Roomba, a consumer-grade autonomous robotic vacuum cleaner, showcased how robots could be integrated into everyday life for practical use. These innovations show rapid advancements in AI, making 2000 the logical post-treatment cut-off for assessing AI’s impact on maternal mortality.
The Difference-in-Differences (DiD) results in Table 3 and Fig. 3 reveal varying AI impacts based on development levels. In developing countries, the treated group had a higher MMR than the control group by 92.04 (113.82) per 100,000 live births for robot stock (flow). However, post-2000, MMR declined relative to pre-2000 levels, suggesting AI’s potential benefits. In developed countries, the treated group and post-2000 period showed lower maternal mortality rates, reinforcing AI’s role in improving maternal health outcomes.
The interaction between treatment and post-treatment periods (treat_post), which captures AI’s actual impact, is significant and negative across all countries and in developing nations (−88.133 and −68.541 globally, −109.83 and −77.37 for developing countries for AI stocks and flows, respectively). This suggests that as AI technologies integrate into healthcare systems, their impact on reducing maternal mortality becomes more pronounced in developing countries over time. These findings align with previous research highlighting AI’s transformative role in improving healthcare access and outcomes in resource-limited settings. AI adoption has a positive but less pronounced effect in developed countries, where maternal mortality rates are already low. The results indicate that greater AI adoption will benefit developing countries, where maternal mortality remains high, and AI implementation is still limited. This supports prior studies emphasizing AI’s long-term benefits in healthcare.
Panel ARDL modelling
Tables 4 and 5 present the panel ARDL model results assessing the impact of AI-driven robotics flow (aiapflow) on maternal mortality (mmr) across all countries, developed and developing countries. The results distinguish between short-run (SR), long-run (LR), and adjustment (ADJ) effects. In Table 6, the adjustment coefficient (ADJ term) for developing countries is significant at 5% and negative (−0.2717), indicating that 27% of deviations from the long-run maternal mortality equilibrium are corrected each period. In developed countries, the ADJ term is also significant and negative at both levels (−0.1336) and log (−0.0701), suggesting a 13.36% or 7.01% correction toward equilibrium per period. However, for all countries combined, the coefficient is positive (0.0488) and not statistically significant, implying weak or no global trend adjustment. These results indicate that maternal mortality in developing countries adjusts toward equilibrium slightly faster than in developed countries following a shock.
Figure 4, depicting the cumulative sum (CUSUM), shows that all variables remain within the 95% confidence band, confirming model stability over time. This is further supported by diagnostic test results in Table 7, indicating that the estimated models are statistically reliable. The Durbin-Watson (DW) statistic suggests minimal autocorrelation, with most values close to 2 (e.g., 2.288, 2.102, 2.218). The Breusch-Godfrey (BG) Chi2 and p-values confirm no significant serial correlation in any model. White’s test results indicate no significant heteroskedasticity, suggesting consistent error variance. Finally, the Pesaran, Shin, and Smith (PSS F-statistics) and p-values confirm cointegration in most models, reinforcing the existence of a stable long-term relationship between AI in robotics and maternal mortality across different countries.
The long-run (LR) effects of AI Robotics Flow indicate a significant negative relationship with maternal mortality across all countries, suggesting that increased AI adoption reduces maternal mortality over time. In developing countries, the effect is stronger and more significant, highlighting a greater long-term impact of AI robotics in reducing maternal mortality. Conversely, in developed countries, the coefficient is positive but insignificant, indicating no strong long-run effect of AI robotics flow on maternal mortality. The negative long-run coefficients in developing countries suggest that AI-driven technologies, particularly in industrial and service robotics, enhance healthcare efficiency and accessibility, ultimately reducing maternal mortality. This aligns with technological diffusion theories, where advanced technologies improve healthcare service delivery, reduce human error, and strengthen maternal health monitoring. The stronger effect in developing countries may reflect a 'technological catch-up' process, where adopting AI-driven innovations enhances healthcare infrastructure, improves medical access, and supports maternal health programs.
The positive short-run effects observed globally and in developing countries suggest transitional disruptions as AI integration initially strains healthcare systems due to high costs, technical challenges, or workforce displacement before long-term benefits emerge. In developed countries, the absence of a significant long-run impact may indicate AI saturation, where additional investments yield diminishing returns on maternal health outcomes due to already advanced healthcare infrastructure. The relationship between AI and maternal health aligns with key economic and public health theories. The innovation and public health theory suggests that technological advancements enhance efficiency and accessibility, improving health outcomes. Meanwhile, the diffusion of innovations theory explains varying impacts across countries, emphasizing how technological adoption stages and contextual factors influence AI’s effectiveness.
Panel ARDL modelling results and discussion for the impact of artificial intelligence (AI) in robotics stock on maternal mortality
Tables 6 and 7 present the panel ARDL (Auto-Regressive Distributed Lag) model results, assessing the impact of AI-driven robotics stock (aiapstock) on maternal mortality across global, developed, and developing countries. Table 8 shows that the adjustment coefficients for maternal mortality are positive and significant, indicating a degree of inertia in maternal mortality rates. This suggests deviations from the long-run equilibrium due to AI robotics stock changes are corrected over time, with a faster adjustment observed in all countries and developing nations. Figure 5, displaying the cumulative sum, reveals that some variables fall outside the 95% confidence band in global and developed country samples. Despite this, the model remains reliable for interpretation. This is further supported by diagnostic test results in Table 8, which confirm that the models are generally well-specified, though minor heteroscedasticity issues exist in some cases. The Durbin-Watson and Breusch-Godfrey tests indicate no significant autocorrelation, ensuring the model’s standard errors remain unbiased. However, White’s test detects heteroscedasticity, particularly in logged models for all countries and developed countries. Importantly, significant PSS F-statistics across all models confirm a long-run relationship between maternal mortality and AI robotics stock, suggesting cointegration. This indicates that maternal mortality and AI advancements move together over time, with deviations from equilibrium corrected in the future. The findings reinforce that AI has long-term implications for maternal mortality reduction across different country groups.
At the global level, AI robotics stock has a statistically significant negative long-run impact on maternal mortality, indicating that expanding AI technologies in industry and services reduces maternal mortality worldwide. A 1-unit increase in AI robotics stock (aiapstock) lowers MMR by 0.0042 units (level) or 0.8390% (log). AI also significantly reduces maternal mortality in the short run, particularly in the log model (0.1158), underscoring its immediate benefits. AI-driven diagnostic tools, automated surgical robots, and improved healthcare delivery contribute to better maternal health outcomes by enhancing obstetric care and addressing complications more effectively.
The long-run impact is mixed for developing countries (see Columns 3 and 4). In the level model, AI robotics stock significantly reduces maternal mortality (0.0108). However, the log model shows no significance, suggesting that while AI stock influences maternal mortality, its effects may not scale logarithmically. In the short run, AI exhibits significant adverse effects at first and second lags, indicating immediate and sustained reductions in maternal mortality. The impact is more pronounced in developing countries, where healthcare access and quality gaps are larger. AI technologies help bridge these gaps by enhancing diagnostics, expanding telemedicine, and improving healthcare efficiency, ultimately reducing maternal mortality rates. However, the insignificance of the log model suggests that AI penetration remains too limited to generate large-scale effects. These findings align with the health production function framework, which views health outcomes as a function of technological inputs. AI robotics enhances healthcare efficiency and service delivery, reinforcing prior studies highlighting AI’s positive role in reducing mortality in developing regions.
For developed countries (see Columns 5 and 6), the long-run impact of AI robotics stock on maternal mortality is insignificant, both in the level and log models, suggesting that AI does not significantly influence maternal mortality over time. This is likely due to already high healthcare standards, where additional AI investments yield diminishing returns. In the short run, several lagged AI robotics stock terms (LD.aiapstock, L2D.aiapstock, L3D.aiapstock) show significant negative coefficients, indicating that AI has a more immediate impact. This suggests cutting-edge AI technologies enhance short-term medical interventions, improving operational efficiency, resource allocation, and emergency maternal healthcare responses. The contrast between developed and developing countries aligns with economic convergence theory, which posits that less developed nations experience greater benefits from adopting advanced technologies. Since developing countries start from a lower healthcare baseline, AI integration has a more pronounced effect on maternal mortality reduction than developed nations.
Fixed effect regression results and discussion for the impact of artificial intelligence (AI) on maternal mortality
For all countries (Columns 1 and 2, Table 8), the AI stock coefficient (−0.00003) is statistically significant at the 5 percent level, indicating that higher AI stock marginally reduces maternal mortality rates. This suggests that accumulated industrial and service robotics improve maternal health outcomes. The AI flow coefficient (−0.00013) is also significant at the 5 percent level, showing a stronger negative impact on maternal mortality rates than AI stock. This implies that advancements in AI, particularly in healthcare services, are more effective in reducing maternal deaths, aligning with previous studies.
For developing countries (Columns 3 and 4), the AI stock coefficient (−0.00005) is significant at the 10 percent level, reinforcing that increased AI stock helps lower maternal mortality, with a slightly larger effect than in the overall sample. AI applications in maternal health services, such as robotic-assisted procedures and diagnostics, can help bridge healthcare infrastructure gaps. The AI flow coefficient (−0.000152) is also significant at the 10 percent level, indicating that new AI technologies more effectively reduce maternal mortality in developing countries by addressing healthcare deficiencies through cost-effective diagnostics and telemedicine solutions. The significant negative coefficients for AI stock and flow suggest that AI technologies can fill critical gaps in maternal healthcare, particularly where access to skilled medical personnel is limited. These findings align with technological leapfrogging theory, which posits that developing nations benefit more from newer technologies than developed countries with established infrastructures.
For developed countries (Columns 5 and 6), the AI stock coefficient (0.000023) and AI flow coefficient (0.000049) are positive but not significant, indicating no clear relationship between AI adoption and maternal mortality rates. This suggests that AI may enhance efficiency but does not significantly impact maternal health outcomes in countries with already advanced healthcare systems.
The global stock of robots tripled to 2.25 million in 2018, with projections estimating 20 million robots by 2030, representing a 19% annual growth rate. This rate is used to extend yearly flows and stocks of industrial and service robots to 2035, though it remains conservative given the 48% increase in professional service robot sales in 2022.
To analyze the impact of AI-driven robotics (AI stock and AI flow) on maternal mortality (MMR), panel fixed-effects models are estimated using actual data from 1993 to 2020 across global, developing, and developed countries. Figure 6 presents forecasts based on fixed-effects (FE) regression models, controlling for health access, obstetric care, and comorbidities while allowing AI indicators (stock and flow) to vary. The forecasts remain reliable, as indicated by the narrow 95% confidence intervals (shaded grey area), particularly in developed countries.
The forecast suggests a slightly more substantial impact of AI flow on maternal mortality (MMR) than AI stock. Globally, MMR follows a clear downward trend in both AI stock and flow models. The actual values (blue line) remained stable from 1990 to 2020. The forecast (red line) projects a significant decline from 2020 onward, with MMR dropping below 20 per 100,000 live births by 2035. The forecast shows a steeper initial decline in developing countries, with MMR falling below 50 by 2030 in both models. However, the decline is more pronounced in the AI flow model compared to AI stock. Furthermore, the forecast predicts a modest further reduction in developed countries, with low MMR (below 20 per 100,000). The AI stock model shows little change beyond 2020, while the AI flow model indicates a slight decline, keeping MMR below 10.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0






















































































































































































