Can Copper in Your Diet Boost Brain Health in Older Adults?
A recent study suggests that increasing dietary copper intake may improve cognitive function in older adults, particularly stroke survivors. Learn about the potential benefits of copper and how it relates to memory and thinking skills.
A large US study suggests that boosting copper in the diet may support sharper thinking in later life, up to a point. Discover how much copper makes a difference, and why stroke survivors might benefit most.
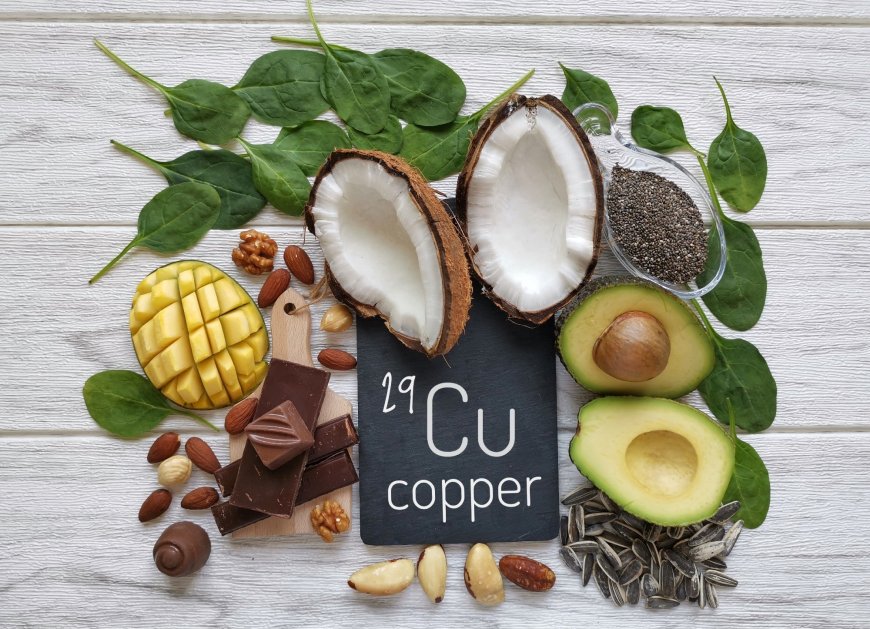
Study: Association between dietary copper intake and cognitive function in American older adults: NHANES 2011–2014. Image Credit: Danijela Maksimovic / Shutterstock
In a recent study published in the journal Scientific Reports, researchers investigated the relationship between copper intake and cognitive function in older adults. All forms of dementia, including mild cognitive impairment and Alzheimer’s disease, are characterized by cognitive decline and are emerging as a global public health concern.
The Global Burden of Disease study has projected that 152.8 million individuals will have dementia by 2050. Exploring protective factors for cognition is vital to preventing cognitive impairment. Of late, micronutrients have received substantial attention for their role in reducing cognitive decline. An imbalance of specific micronutrients in the brain, such as selenium, copper, and zinc, is reportedly linked to cognitive decline and neurodegenerative diseases.
Copper is vital for several physiological functions. It is a cofactor for enzymes involved in cellular energy production, antioxidant defenses, and neurotransmitter synthesis. However, both deficiency and excess can be neurotoxic due to copper's role in oxidative stress pathways. Nonetheless, the relationship between cognition and copper remains poorly understood.
About the study
Researchers carefully accounted for other dietary components, adjusting models not just for energy intake but also levels of zinc, iron, selenium, fat, and saturated fatty acids alongside copper.
In the present cross-sectional observational study, researchers investigated the association between dietary copper intake and cognitive function in older adults in the United States. Participants of the National Health and Nutrition Examination Survey (NHANES) from 2011 to 2014 were included. Individuals under 60 years and lacking information on cognitive tests, copper intake, or covariates were excluded. NHANES used a 24-hour dietary recall questionnaire to collect information on the intake of all food types within the past 24 hours.
Participants were eligible for two dietary recall interviews. Copper intake was determined from dietary recall data and categorized into quartiles: Q1 (<0.76 mg/day), Q2 (0.76–1.04 mg/day), Q3 (1.05–1.43 mg/day), and Q4 (≥1.44 mg/day). Participants underwent various assessments of cognitive function. These include the delayed and immediate verbal list learning tests (CERAD-DRT and CERAD-IRT), the digit symbol substitution test (DSST; assessing processing speed), and the animal fluency test (AFT; assessing verbal fluency).
A global cognitive Z score was calculated as the mean of the standardized scores of the four cognitive tests, with higher scores indicating superior cognitive performance. The baseline characteristics of the participants were compared using the chi-squared test and analysis of variance (ANOVA).
For stroke survivors, the cognitive boost from higher copper was notably stronger, with their global cognitive score showing a sharper rise compared to those without a stroke history.
Multivariate linear regression models were used to assess the relationship between cognitive function and copper intake. Model 1 was not adjusted for any confounding variable, whereas model 2 was adjusted for age, race, gender, marital status, education, and poverty income ratio (PIR).
Model 3 was further adjusted for body mass index (BMI), alcohol status, smoking status, and history of stroke, diabetes, hypertension, or cardiovascular disease. Model 4 was additionally adjusted for dietary energy, iron, selenium, fat, zinc, and total saturated fatty acids.
Furthermore, a generalized additive model was used to account for the nonlinear relationship between copper intake and cognitive test scores. In addition, subgroup analyses were performed by age, gender, BMI, hypertension, coronary heart disease, stroke, and diabetes.
Findings
Copper's potential brain benefits may stem partly from its role in making acetylcholine, a key neurotransmitter for learning and memory highlighted in the paper's discussion.
The study included 2,420 participants, with a mean age of 69.3 years and a BMI of 29.2 kg/m². Most participants were female (50.9%), non-Hispanic White (50.2%), and married or cohabiting (58.3%). Participants with higher copper intake were more likely to be male, non-Hispanic White, and have lower smoking rates and higher family income, compared to those with low copper intake. Further, individuals with higher copper intake had higher scores on cognitive tests.
Dietary copper intake was positively associated with cognitive test scores. In the fully adjusted model, participants in the highest quartile (Q4: ≥1.44 mg/day) of copper intake showed significantly higher scores in DSST, AFT, CERAD-DRT, and global cognition, but not in CERAD-IRT (immediate recall). Cognitive test scores increased with an increase in copper intake. These associations remained significant after adjusting for various covariates.
Notably, an inverse, L-shaped relationship was observed between copper intake and DSST, AFT, and global cognitive Z scores, but no nonlinear relationship was found for the CERAD immediate or delayed recall tests. The relationship was no longer significant beyond specific inflection points (1.22 mg/day for the global cognitive Z score, 1.42 mg/day for AFT, and 1.63 mg/day for DSST).
Subgroup analyses showed that increased copper intake was associated with a higher global cognitive Z score, specifically in individuals with a history of stroke, potentially due to copper's role in reducing post-stroke inflammation and promoting neuronal repair.
Conclusions
In sum, dietary copper intake was associated with superior cognitive function in older adults. The association was sustained after adjusting for various confounding variables. There was a L-shaped relationship between dietary copper intake and processing speed (DSST), verbal fluency (AFT), and global cognition, with the association being insignificant beyond specific thresholds. However, this observational study cannot prove causality, and self-reported dietary data and residual confounding may limit findings. Further longitudinal analyses are needed to corroborate these findings.
According to the source: News-Medical.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0
















































































































































































